Blog - Fort Wayne, IN
Tips, Facts, And The
Latest In Dentistry

Bone Graft and Implant: Is it Always Needed?
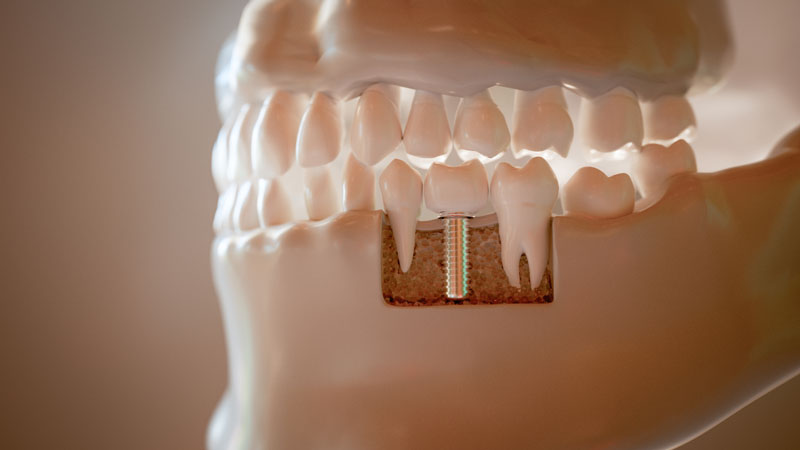
A bone graft implant refers to adding bone material to the jaw before or during placement of a dental implant. The central question many patients ask is simple: is a bone graft always needed for dental implants? This article explains when grafting is recommended, what types of grafts exist, alternatives, risks, and how clinicians decide. You’ll get clear guidance so you can talk with your dentist or implant specialist with confidence.
Not every implant needs a graft. In many cases implants can be placed without extra bone work, but when bone is missing or weak, a bone graft implant may be the safest route for long-term stability and function.
When is a bone graft implant actually needed?
Bone loss after tooth removal, long-term dentures, infection, or trauma can leave the jaw too thin or short to hold an implant securely. Without enough bone, an implant can fail or lead to poor looks and chewing ability. Clinicians use a combination of a clinical exam and CBCT imaging to decide whether a bone graft implant is required.
Common causes of insufficient bone
- History of tooth extraction without immediate implant placement
- Advanced periodontal (gum) disease
- Facial trauma or injury
- Long-term missing tooth or prolonged denture use
How clinicians assess the need
Assessment centers on imaging and measurements:
- CBCT (cone beam CT) gives a 3D view of bone height, width, and quality.
- Measurements of bone width and height determine if an implant of adequate size will fit.
- Implant planning software is used to simulate implant placement and predict how much bone support is needed.
- Clinical exam checks gum health, bite forces, and soft tissue thickness.
Types of bone grafts and timing with implants
There are several graft materials and choices depend on the defect size, location, and patient factors.
- Autograft: Bone taken from the patient (chin, ramus, or hip). Best for healing but requires an extra surgical site.
- Allograft: Donor human bone processed for safety. Common and avoids a second surgery.
- Xenograft: Animal-derived bone (usually bovine). Often used as a scaffold to support new bone growth.
- Synthetic (alloplast): Man-made materials like calcium phosphate. Good for many routine cases.
Simultaneous vs staged graft and implant placement
A graft and implant can sometimes be done at the same time when there’s enough remaining bone for good primary stability. This shortens treatment time. A staged approach—graft first, place implant after healing (often 3–6 months)—is safer when the defect is large or stability cannot be achieved immediately. Sinus lifts are often staged when significant vertical bone gain is needed in the upper back jaw.
Alternatives, risks, and recovery
For some patients, alternatives to a traditional bone graft implant exist:
- Short or narrow implants when vertical bone is limited
- Angled implants to use available bone without grafting
- Zygomatic implants for severe upper jaw bone loss (specialized option)
- Mini implants for temporary or specific low-load situations
The right alternative depends on location, bite forces, and long-term goals.
Risks and what to expect after a graft implant procedure
Common risks include infection, swelling, graft failure, or delayed healing. Most patients experience some soreness and swelling for a few days. Typical healing for a graft before implant placement ranges from 3 to 6 months depending on the graft type and site.
Call your dentist if you notice persistent fever, increasing pain after the first few days, excessive swelling, drainage from the site, or a loose implant or graft material.
How to decide and next steps
Choosing whether you need a bone graft implant is a personalized decision. Your implant dentist or specialist will weigh:
- Oral and overall health (smoking, diabetes, medications)
- Bone quantity and quality from CBCT imaging
- Desired timeline and budget
- Long-term restoration goals and esthetics
A clear treatment plan requires an exam and 3D imaging. Speak with an experienced implant dentist for a tailored plan and an imaging-based estimate. To move forward, schedule a consult to review your CBCT, options, risks, and a recommended timeline.
Ready to learn if a bone graft implant is right for you? Book a consult with an implant specialist to get a personalized plan and next steps based on your imaging and goals.